A substantial subset of follicular lymphoma (FL) patients has an early relapse with a poor outcome. We showed that this unfavorable group displays increased expression of IRF4, dysregulated immune signaling and an immunosuppressive microenvironment. At the molecular level, IRF4 controls expression of antigen presentation and immune molecules (e.g. HLA-DR, CD40, PDL1). Furthermore, silencing of IRF4 triggers anti-lymphoma immunity ( Mondello P et al, Blood 2022;140 Suppl 1:168-169). However, little is known on the molecular mechanisms whereby IRF4 controls the crosstalk between B and T cells.
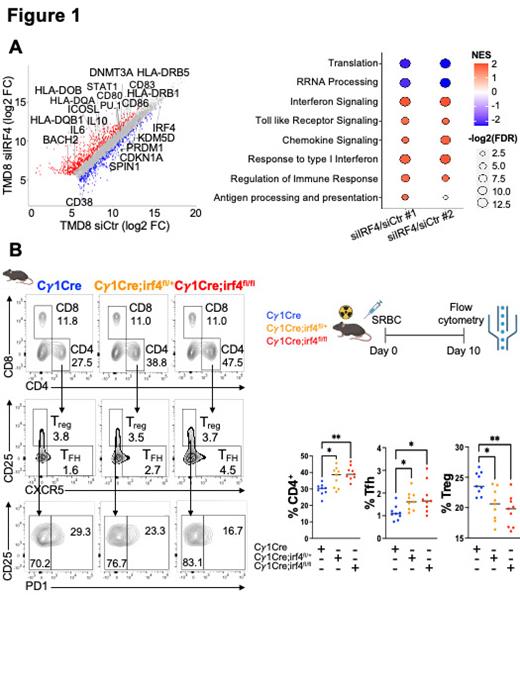
To address this question, first we performed RNA-seq, ATAC-seq and CUT&TAG of active (H3K27Ac, H3K4me3) and repressive (H3K27me3, H3K4me1) histone marks in TMD8 and HBL1 (lymphoma cells with high IRF4 expression) transfected with two pairs of siIRF4 or siCtr for 72 hours. Gene expression revealed a broad change in transcription, with 432 upregulated genes and 136 downregulated genes in siIRF4 compared to siCtr. Notably, the genes with increased expression following IRF4 silencing coded for antigen presentation, immune molecules and cytokines (e.g. HLA-DR, CD86, IL6, IL10). Accordingly, we observed significant enrichment of antigen presentation, interferon and immune response signatures ( Fig 1A). Integrating RNA-seq with chromatin accessibility showed a significant shift towards transcriptional upregulation at genes nearest to upregulated ATAC peaks, with significant enrichment at enhancers (n=771). Conversely, transcriptional suppression was enriched at enhancers (n=2,458) of downregulated peaks. k-means analyses of all union peaks, generated by merging ATAC with CUT&TAG peaks, revealed a significant gain of H3K4me3, with concordant loss of H3K4me1 at enhancers with upregulated gene expression. In contrast, H3K4me3 was severely decreased at suppressed peaks. TF motif analysis revealed an enrichment for PU.1 and E2A at IRF4-bound regions, suggesting their cooperation in regulating immune signaling.
Since antigen presentation and other immune molecules are critical components of the immune synapse, we explored the role of IRF4 on the interaction between germinal center (GC) B and T cells by crossing irf4 fl/fl mice with conditional deletion of irf4 ( Klein et al, Nat Immunol 2006) and Cγ 1cre mice ( Cγ 1cre; irf4 fl/fl) to induce recombination in GC B cells. After 10 days of immunization (GC reaction peak), Cγ 1cre; irf4 fl/fl and Cγ 1cre; irf4 fl/+ GC B cells showed significant increase of HLA-DR and CD40 expression compared to WT. As expected, Cγ 1cre; irf4 fl/fl mice displayed a significantly skewed light-zone:dark-zone ratio in favor of increased dark-zone, which are the cells that most reflect the action of BCL6, with concordant suppression of plasma cells. Additionally, we observed a significant increase of CD4 + T cells after partial or complete deletion of irf4, with upregulation of T FH cells and decrease of T reg cells ( Fig 1B). Notably, mice with loss of irf4 showed a significant decrease in exhausted T FH cells. To test if this effect was dependent on MHC:TCR interaction, we cocultured CD4 + T cells with TMD8 cells transfected with two siIRF4 or siCtr in presence of blocking antibodies for MHC class I, MHC class II or both. Blocking one or the other MHC class I or II partially rescued the IRF4 effect on T reg and T FH cells respectively as well as reduced anti-lymphoma cytotoxicity. Further experiments blocking IRF4-dependent IL6 and IL10 identified these two cytokines as responsible for the additional effects on T cells. To confirm this as an antigen-dependent immune response we coculture sorted GC B cells from NP-OVA-immunized Cγ 1cre; irf4 fl/fl, Cγ 1cre; irf4 fl/+ and WT mice with CSFE-labeled OVA-specific OT-II CD4 + T cells at a ratio of 2:1 in an organoid system for 5 days. We observed induced antigen specific proliferation of CD4 + T cells in the presence of Cγ 1cre; irf4 fl/fl and Cγ 1cre; irf4 fl/+ GC B cellscompared to WT,as indicated by decrease in CSFE expression . We confirmed an increase of T FH cells and a decrease of T reg cells, supporting the conclusion that IRF4 directly controls the antigen-dependent immune response .
In summary, IRF4 expression in GC and lymphoma B cells regulates immune signaling with PU.1 and E2A, thereby modulating antigen-dependent immune responses with potential implications for lymphomagenesis. Future studies investigating targeting of IRF4 in lymphoma are warranted.
Disclosures
Ansell:ADC Therapeutics, Affimed, Bristol-Myers Squibb Company, Pfizer Inc, Regeneron Pharmaceuticals Inc, Seagen Inc, Takeda Pharmaceuticals USA Inc.: Other: Contracted Research.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal